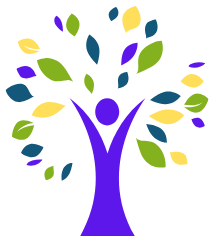
Natural Seasonal Allergies: Causes, Symptoms, and Effective Remedies
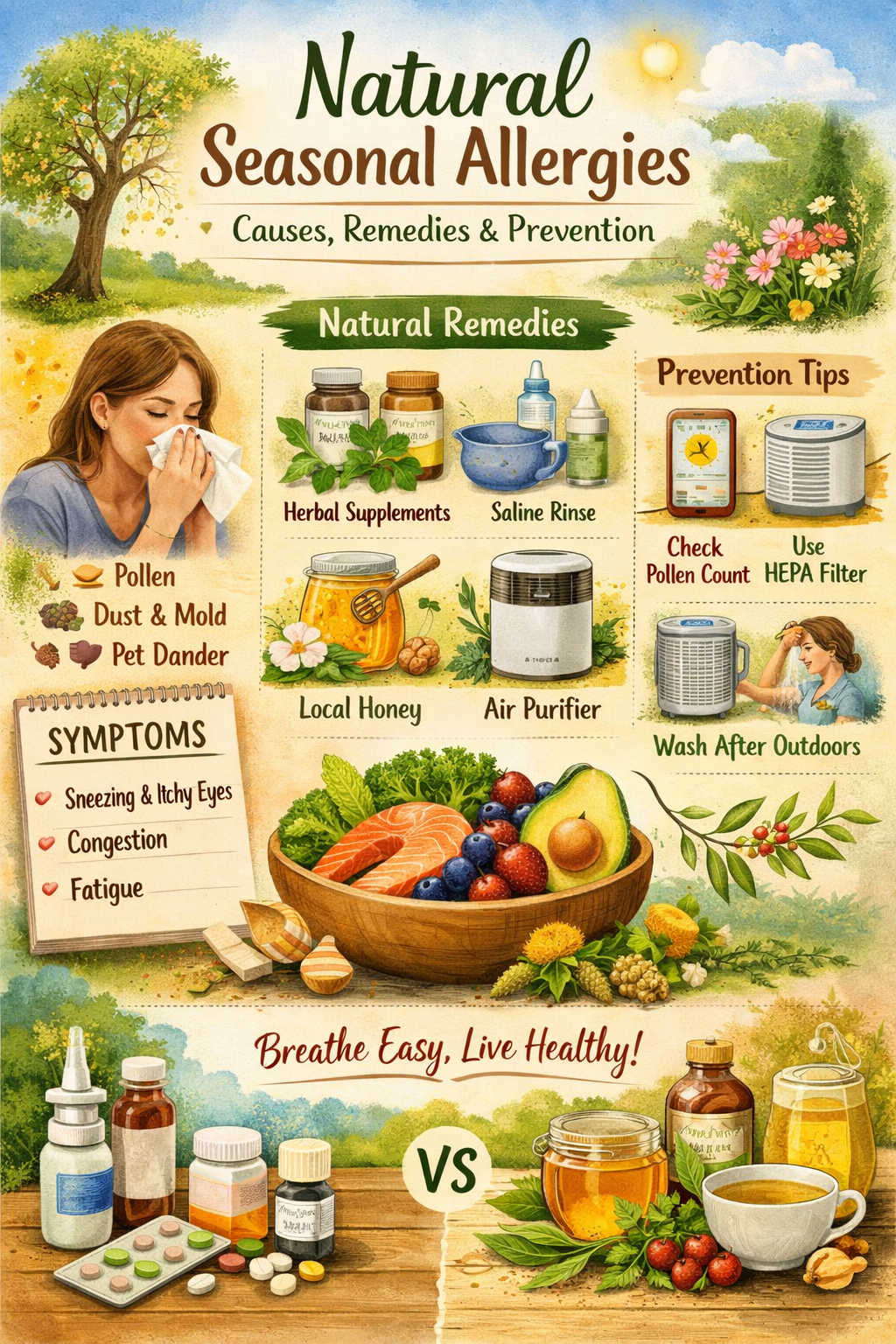
Seasonal changes bring beauty and new beginnings, but for millions of people worldwide, they also bring natural seasonal allergies—unpleasant symptoms triggered by pollen, mold, and other environmental allergens. Unlike chronic allergies that persist year-round, seasonal allergies appear during specific times of the year, often in spring, summer, or fall. These allergies can significantly affect your quality of life, causing sneezing, itchy eyes, congestion, fatigue, and even sleep disturbances.
Understanding natural seasonal allergies is essential to managing them effectively. By learning the causes, common triggers, and natural remedies, you can reduce symptoms without relying solely on medication.
What Are Seasonal Allergies?
Seasonal allergies, also called hay fever or allergic rhinitis, are immune system reactions that occur when the body overreacts to allergens present in the environment. These allergens are typically harmless to most people but can trigger symptoms in sensitive individuals. Common triggers include pollen from trees, grasses, and weeds, as well as mold spores and dust.
Unlike chronic allergies, which persist year-round, seasonal allergies appear only during certain times, usually when specific plants release pollen. For example:
- Spring: Tree pollen, especially from birch, cedar, and oak
- Summer: Grass pollen, such as ryegrass, Bermuda grass, and Timothy grass
- Fall: Weed pollen, particularly ragweed
Environmental factors such as air pollution, humidity, and wind can worsen allergy symptoms by spreading allergens more widely. Seasonal allergies can affect anyone, but people with a family history of allergies, asthma, or eczema are more prone to developing them.
Symptoms can range from mild discomfort to severe reactions that interfere with daily life. Common signs include sneezing, runny nose, itchy eyes, congestion, sinus pressure, and fatigue. While conventional medications like antihistamines are widely used, many people prefer natural remedies for seasonal allergies, including lifestyle adjustments, herbal supplements, and dietary changes.
Key Takeaways:
| Feature | Seasonal Allergies |
|---|---|
| Timing | Appear during specific seasons |
| Common Triggers | Pollen, mold, dust, weeds |
| Symptoms | Sneezing, congestion, itchy eyes, fatigue |
| Risk Factors | Family history, asthma, eczema |
| Treatment Options | Natural remedies, lifestyle changes, medications |
By understanding what triggers natural seasonal allergies, you can take proactive steps to manage your symptoms, minimize exposure, and maintain a healthy, allergy-free lifestyle.
Causes of Natural Seasonal Allergies
Understanding the causes of natural seasonal allergies is the first step toward preventing and managing symptoms effectively. Seasonal allergies occur when the body’s immune system mistakenly identifies harmless substances in the environment as threats. This overreaction triggers the release of chemicals like histamine, which leads to the familiar symptoms of sneezing, itching, and congestion.
Pollen and Plant-Based Triggers
Pollen is the most common culprit behind seasonal allergies. Different types of pollen dominate different seasons:
- Tree pollen (Spring): Trees such as birch, cedar, oak, and maple release pollen in spring. Even brief exposure outdoors can trigger sneezing and watery eyes.
- Grass pollen (Summer): Grasses like Bermuda, Timothy, and ryegrass produce pollen in late spring and summer. People sensitive to grass pollen often experience congestion and itchy eyes.
- Weed pollen (Fall): Ragweed is the primary culprit during fall. A single ragweed plant can release up to a billion pollen grains per season, causing widespread allergic reactions.
Pollen counts fluctuate depending on weather conditions. Windy, dry days can spread pollen widely, while rainy or humid conditions may temporarily reduce pollen exposure. Monitoring local pollen forecasts can help individuals plan outdoor activities and minimize contact with allergens.
Environmental Factors
Besides pollen, several environmental elements contribute to natural seasonal allergies:
- Air pollution: Particles from vehicles and factories can aggravate the respiratory system, making it more reactive to allergens.
- Weather changes: Sudden temperature swings or windy conditions can trigger allergy flare-ups.
- Indoor allergens: Dust mites, pet dander, and mold spores can intensify seasonal symptoms when they infiltrate homes, especially during peak pollen months.
Genetic and Personal Factors
Some people are genetically predisposed to allergies. If you have a family history of allergic conditions like asthma, eczema, or hay fever, your chances of developing seasonal allergies are higher. Additionally, a weakened or hyperactive immune system can overreact to minor allergens, leading to more severe symptoms.
Quick Facts About Causes of Seasonal Allergies:
- Over 50 million people in the U.S. experience seasonal allergies each year (Source: AAAAI).
- Ragweed pollen can travel up to 400 miles on the wind.
- Genetics account for 30–50% of an individual’s susceptibility to allergies.
Understanding these causes is crucial because it allows you to take preventive measures, such as limiting exposure during high-pollen days, improving indoor air quality, and using natural supplements that support the immune system.
Symptoms of Natural Seasonal Allergies
Recognizing the symptoms of natural seasonal allergies early is essential for managing them effectively. These symptoms occur because the body’s immune system reacts to allergens by releasing chemicals such as histamine, which triggers inflammation in the nasal passages, eyes, and respiratory system. While symptoms vary in severity, they can significantly affect daily life if left unmanaged.
Common Physical Symptoms
People with natural seasonal allergies often experience a combination of the following symptoms:
- Sneezing and runny nose: Frequent sneezing and clear nasal discharge are hallmark signs of seasonal allergies.
- Itchy, watery eyes: Pollen irritates the eyes, causing redness, swelling, and constant itching.
- Nasal congestion and sinus pressure: Blocked nasal passages can lead to difficulty breathing and sinus headaches.
- Coughing and throat irritation: Postnasal drip from excess mucus often causes throat irritation and mild coughing.
- Fatigue and irritability: Persistent allergy symptoms can disrupt sleep and lead to tiredness and mood swings.
- Skin reactions: Some individuals may develop rashes, hives, or eczema flare-ups when exposed to allergens.
Less Obvious Symptoms
Not all symptoms are immediately linked to allergies, but awareness is important:
- Headaches: Sinus pressure and congestion may cause mild to moderate headaches.
- Difficulty concentrating: Brain fog or difficulty focusing can result from sleep disturbances caused by nasal congestion.
- Ear discomfort: Allergic inflammation can block the Eustachian tubes, causing a feeling of fullness or popping in the ears.
When to Seek Medical Advice
While natural remedies can alleviate most symptoms, medical attention is necessary if:
- Symptoms are severe or worsening despite preventive measures.
- You experience shortness of breath, wheezing, or asthma attacks.
- Allergic reactions interfere with daily life or sleep consistently.
Quick Symptom Checklist for Natural Seasonal Allergies:
| Symptom | Description |
|---|---|
| Sneezing | Frequent and repetitive sneezing fits |
| Runny nose | Clear nasal discharge |
| Itchy eyes | Redness, watering, or puffiness in eyes |
| Congestion | Blocked nasal passages, sinus pressure |
| Fatigue | Sleep disturbances and tiredness |
| Skin reactions | Rashes, hives, or eczema flare-ups |
| Headache & brain fog | Caused by sinus inflammation and poor sleep |
| Ear discomfort | Pressure or fullness in ears |
Diagnosing Natural Seasonal Allergies
Proper diagnosis is key to managing natural seasonal allergies effectively. While many people self-diagnose based on symptoms, identifying the specific allergens causing your reaction can help you choose the best natural remedies and preventive strategies.
Allergy Testing Options
There are several ways to diagnose seasonal allergies medically:
- Skin Prick Test:
- Small amounts of common allergens (pollen, mold, dust, pet dander) are introduced into the skin.
- A positive reaction—redness or swelling—indicates sensitivity.
- Results are available within 15–20 minutes.
- Blood Test (IgE Test):
- Measures the level of allergy-specific antibodies in your blood.
- Useful for individuals with skin conditions or those taking medications that interfere with skin tests.
- Can identify multiple allergens at once.
These tests allow for a precise understanding of which allergens trigger your symptoms, helping you tailor natural remedies and lifestyle adjustments.
Tracking Symptoms Naturally
Even without medical testing, you can track and identify seasonal allergy triggers naturally:
- Symptom Diary: Record daily symptoms, noting time of day, location, and possible exposures.
- Pollen Count Monitoring: Check local pollen forecasts to see if symptoms align with high pollen days.
- Environmental Observations: Note triggers like outdoor activities, cleaning routines, or pet exposure.
Keeping track of your symptoms helps you correlate allergic reactions with specific allergens, making prevention and natural treatment more effective.
Case Study: Natural Symptom Tracking
Jane, a 32-year-old teacher, noticed sneezing and itchy eyes every April. By keeping a symptom diary and checking pollen counts, she identified birch tree pollen as the main trigger. With this information, she started using saline nasal rinses, air purifiers, and herbal supplements during peak months, which significantly reduced her symptoms without daily medication.
Key Takeaways for Diagnosis:
- Proper diagnosis ensures more targeted management of seasonal allergies.
- Skin and blood tests provide precise allergen identification.
- Natural symptom tracking empowers you to prevent and treat allergies proactively.
Natural Remedies for Seasonal Allergies
For those seeking relief without relying solely on medications, natural remedies for seasonal allergies can be highly effective. These remedies work by reducing exposure to allergens, calming the immune response, and supporting overall respiratory and immune health.
Lifestyle Changes to Reduce Allergy Exposure
Simple adjustments to daily routines can make a significant difference:
- Monitor pollen levels: Stay indoors on high-pollen days, especially during mornings and windy conditions.
- Close windows and doors: Prevent pollen from entering your home during peak seasons.
- Shower and change clothes after outdoor exposure: Pollen sticks to hair, skin, and clothing.
- Use air purifiers: HEPA filters remove airborne allergens inside your home.
- Regular cleaning: Vacuum carpets and dust surfaces to reduce indoor allergens.
Tip: Wearing sunglasses outdoors can protect your eyes from pollen irritation, while a mask can reduce nasal exposure.
Natural Supplements for Seasonal Allergies
Certain vitamins and plant-based compounds can help modulate the immune system and reduce allergy symptoms:
- Quercetin: A plant flavonoid found in onions, apples, and berries; acts as a natural antihistamine.
- Vitamin C: Supports immune function and may reduce histamine levels.
- Bromelain: An enzyme from pineapple that can reduce nasal swelling and congestion.
- Probiotics: Promote gut health, which plays a role in immune regulation.
- Local honey: May expose the body to small amounts of local pollen, potentially reducing sensitivity over time (though research is mixed).
Case Study: A small study published in the Journal of Allergy and Clinical Immunology found that quercetin supplementation reduced sneezing and nasal congestion in participants with seasonal allergies after four weeks.
Herbal Remedies for Seasonal Allergies
Herbs can be a gentle and effective way to manage allergy symptoms naturally:
- Butterbur: Shown to reduce nasal symptoms in clinical trials.
- Stinging nettle: Acts as a natural antihistamine; can be consumed as tea or capsule.
- Elderberry: Supports immune health and may reduce inflammation.
- Chamomile: Can be used as tea or inhalation for mild relief of congestion.
- Peppermint and eucalyptus: Steam inhalation with these herbs can open nasal passages and soothe irritation.
Nasal and Home Remedies
Targeting allergens directly at the nasal passages and respiratory system is often highly effective:
- Saline nasal rinses: Flush out pollen and reduce nasal inflammation.
- Steam inhalation: Moistens airways and relieves congestion.
- Cold compresses: Reduce eye irritation caused by pollen exposure.
- Humidifiers: Maintain optimal indoor humidity to prevent dryness and irritation.
Quick Summary of Natural Remedies for Seasonal Allergies:
| Type | Examples | Benefits |
|---|---|---|
| Lifestyle | Pollen monitoring, air purifiers, cleaning routines | Reduces allergen exposure |
| Supplements | Quercetin, Vitamin C, Bromelain, Probiotics | Supports immune system, reduces histamine |
| Herbs | Butterbur, Stinging nettle, Chamomile | Natural antihistamines, anti-inflammatory |
| Home Remedies | Saline rinses, steam inhalation, cold compresses | Relieves nasal and eye symptoms |
By combining lifestyle adjustments, dietary supplements, herbal remedies, and home practices, most people can significantly reduce the impact of natural seasonal allergies without heavy reliance on medication.
Diet and Nutrition to Reduce Allergy Symptoms
What you eat can have a significant impact on natural seasonal allergies. Certain foods can support the immune system, reduce inflammation, and help your body respond more effectively to allergens, while others may worsen symptoms. By making strategic dietary choices, you can complement other natural remedies for seasonal allergies.
Anti-Inflammatory Foods
Incorporating anti-inflammatory foods can help calm the body’s overactive immune response to allergens:
- Fruits: Berries, oranges, kiwis, and pineapple are high in antioxidants and vitamin C, which may reduce histamine levels.
- Vegetables: Leafy greens, broccoli, and bell peppers provide essential vitamins and minerals to support immune health.
- Omega-3 Rich Foods: Fatty fish like salmon, sardines, and mackerel, as well as flaxseeds and chia seeds, can reduce inflammation in the nasal passages and respiratory system.
Foods to Avoid During Allergy Season
Certain foods can aggravate allergy symptoms or worsen inflammation:
- Dairy products: Milk, cheese, and cream may increase mucus production in some individuals.
- Refined sugars and processed foods: Can promote inflammation and weaken immune response.
- Alcohol and caffeine (in excess): May dehydrate the body, leading to thicker mucus and congestion.
Hydration for Allergy Relief
Proper hydration is essential for reducing congestion and supporting overall respiratory health:
- Drink plenty of water throughout the day to keep mucus thin and nasal passages moist.
- Herbal teas, such as chamomile, peppermint, or ginger, can also soothe irritation and reduce inflammation.
Case Study: Nutrition and Allergy Management
Mark, a 45-year-old software engineer, struggled with severe seasonal allergies every spring. After consulting a nutritionist, he incorporated anti-inflammatory foods like berries, leafy greens, and salmon into his diet while reducing dairy and processed sugars. Within two months, his sneezing, congestion, and eye irritation decreased significantly, complementing his use of natural remedies like saline rinses and herbal teas.
Quick Tips for Allergy-Friendly Eating
- Eat a variety of colorful fruits and vegetables daily.
- Include omega-3 fatty acids in meals at least 3 times a week.
- Avoid processed foods, refined sugars, and excessive dairy during peak allergy seasons.
- Drink 8–10 glasses of water daily to stay hydrated.
- Consider herbal teas with natural anti-inflammatory properties.
Preventing Natural Seasonal Allergies
Prevention is often the most effective way to manage natural seasonal allergies. By taking proactive measures, you can significantly reduce symptoms and improve overall comfort during allergy seasons.
Plan Outdoor Activities According to Pollen Forecasts
- Check daily pollen counts in your area using weather apps or local allergy forecasts.
- Limit outdoor exposure during peak pollen times, typically early mornings and windy days.
- If outdoor activity is unavoidable, wear sunglasses and a pollen mask to minimize contact with allergens.
Maintain a Clean Indoor Environment
- Keep windows and doors closed during high pollen days to prevent allergens from entering your home.
- Vacuum carpets and rugs regularly using a vacuum with a HEPA filter.
- Clean bedding weekly in hot water to remove dust mites and pollen.
- Use air purifiers with HEPA filters in bedrooms and living spaces to trap airborne allergens.
Pet Care Tips to Reduce Allergens
- Bathe and brush pets regularly to minimize dander.
- Keep pets out of bedrooms and off furniture to reduce allergen exposure in sleeping areas.
- Wash pet bedding frequently.
Personal Hygiene Practices
- Shower and change clothes after spending time outdoors. Pollen can stick to hair, skin, and clothing.
- Avoid rubbing your eyes if they are itchy, as this can worsen irritation.
- Use saline nasal sprays after outdoor exposure to flush out pollen.
Lifestyle Adjustments
- Exercise indoors during high pollen days.
- Dry laundry indoors to prevent pollen from sticking to sheets and clothing.
- Stay hydrated to keep nasal passages clear and reduce congestion.
Quick Prevention Checklist
| Prevention Strategy | Action |
|---|---|
| Outdoor planning | Avoid high-pollen times, wear masks & sunglasses |
| Indoor environment | Use HEPA filters, vacuum, clean bedding |
| Pet care | Regular baths, limit bedroom access |
| Personal hygiene | Shower after outdoor exposure, saline rinses |
| Lifestyle adjustments | Exercise indoors, dry laundry indoors, stay hydrated |
Natural vs. Conventional Allergy Treatments
When managing natural seasonal allergies, people often face a choice between natural remedies and conventional medications. Understanding the benefits and limitations of each approach helps you create a safe and effective allergy management plan.
Conventional Allergy Treatments
Conventional treatments are widely used and can provide rapid relief from allergy symptoms:
- Antihistamines: Reduce sneezing, itching, and runny nose by blocking histamine, the chemical responsible for allergy symptoms. Examples include loratadine and cetirizine.
- Decongestants: Help relieve nasal congestion by shrinking blood vessels in the nasal passages. Examples include pseudoephedrine and phenylephrine.
- Nasal corticosteroids: Reduce inflammation in nasal passages, effective for moderate to severe symptoms. Examples include fluticasone and mometasone.
- Allergy shots (immunotherapy): Gradually desensitize the immune system to specific allergens over time.
Pros:
- Fast-acting relief, especially for severe symptoms
- Clinically tested and widely available
- Useful in acute allergy flare-ups
Cons:
- Potential side effects, including drowsiness, insomnia, or increased blood pressure
- Long-term use may not address root causes
- Doesn’t provide immune system support or overall prevention
Natural Remedies for Seasonal Allergies
Natural approaches focus on prevention, symptom management, and immune support:
- Herbal supplements: Butterbur, stinging nettle, and elderberry act as natural antihistamines.
- Lifestyle changes: Air purifiers, pollen monitoring, and hygiene practices reduce exposure.
- Dietary adjustments: Anti-inflammatory foods, probiotics, and hydration support immune health.
- Home remedies: Saline nasal rinses, steam inhalation, and cold compresses alleviate symptoms naturally.
Pros:
- Fewer side effects than conventional medications
- Focuses on prevention and long-term immune support
- Can complement medications for a holistic approach
Cons:
- May take longer to notice results
- Effectiveness varies by individual
- Some remedies, like local honey or herbal supplements, lack large-scale clinical evidence
When to Combine Natural and Conventional Approaches
- People with mild to moderate allergies often benefit from natural remedies alone.
- Those with severe or persistent symptoms may combine conventional treatments (like antihistamines or nasal sprays) with natural strategies for better overall management.
- Consultation with an allergist or healthcare professional ensures safe integration of natural and conventional treatments.
Quick Comparison Table
| Treatment Type | Benefits | Limitations |
|---|---|---|
| Conventional Medications | Fast relief, clinically tested | Side effects, doesn’t address root cause |
| Natural Remedies | Supports immune system, fewer side effects | Slower results, effectiveness varies |
| Combination Approach | Comprehensive management, balances relief and prevention | Requires guidance for safe use |
Common Myths About Natural Seasonal Allergies
There are many misconceptions surrounding natural seasonal allergies, which can lead to ineffective treatment or unnecessary worry. Understanding the facts helps you manage symptoms more effectively.
Myth 1: Allergies Only Happen in Spring
- Reality: While spring is a common season for tree pollen, allergies can occur in any season.
- Summer: Grass pollen triggers symptoms.
- Fall: Ragweed and mold spores are common culprits.
- Winter: Indoor allergens like dust mites and pet dander may cause reactions.
- Seasonal allergies are linked to specific environmental triggers, not just the calendar.
Myth 2: Local Honey Cures All Allergies
- Reality: While local honey may contain trace amounts of pollen, there’s limited scientific evidence that it can fully prevent or cure allergies.
- It may provide mild relief for some, but it should be combined with other natural remedies and preventive measures.
Myth 3: Natural Remedies Work Instantly
- Reality: Herbal supplements, dietary changes, and lifestyle adjustments take time to show results.
- Consistency is key; for example, it may take weeks of using butterbur or quercetin before symptoms noticeably improve.
Myth 4: Allergies Are Always Mild and Harmless
- Reality: Seasonal allergies can cause significant discomfort and may worsen asthma, sinus infections, or sleep quality.
- Severe reactions require prompt attention and may need medical intervention alongside natural management.
Myth 5: Avoiding All Outdoor Activities Prevents Allergies Completely
- Reality: While reducing exposure helps, completely avoiding outdoor activity is impractical.
- Combining preventive measures, lifestyle changes, and natural remedies is more effective for long-term relief.
FAQs About Natural Seasonal Allergies
1. Can natural remedies completely cure seasonal allergies?
Answer: No, natural remedies cannot cure seasonal allergies entirely. They help manage symptoms, reduce inflammation, and support the immune system. Combining natural strategies with preventive measures can significantly improve quality of life.
2. How long do seasonal allergy symptoms last?
Answer: Symptoms typically last as long as allergens are present. For example:
- Spring tree pollen: 4–6 weeks
- Summer grass pollen: 6–8 weeks
- Fall ragweed: 4–5 weeks
Symptoms may subside once allergen exposure decreases.
3. Are natural supplements safe for children and pregnant women?
Answer: Many supplements, such as quercetin, vitamin C, and probiotics, are generally safe, but it’s important to consult a healthcare professional before use, especially for children, pregnant, or breastfeeding women.
4. When should I see an allergist?
Answer: Seek professional help if:
- Symptoms are severe or persistent
- Over-the-counter remedies are ineffective
- You experience asthma symptoms, shortness of breath, or severe sinus infections
5. Can diet really influence seasonal allergies?
Answer: Yes, an anti-inflammatory diet rich in fruits, vegetables, omega-3s, and hydration can reduce inflammation and improve the body’s response to allergens. Avoiding processed foods, refined sugar, and excessive dairy may also help.
6. Are seasonal allergies genetic?
Answer: Genetics play a significant role. If you have a family history of asthma, eczema, or hay fever, you are more likely to develop seasonal allergies. Environmental factors and immune system sensitivity also contribute.
7. What are the safest natural remedies for quick relief?
Answer: Some of the safest options include:
- Saline nasal rinses
- Steam inhalation
- Herbal teas like chamomile or peppermint
- Quercetin or butterbur supplements (with proper dosage)
Conclusion
Natural seasonal allergies affect millions of people worldwide, causing discomfort, fatigue, and disruption in daily life. Understanding the causes, triggers, and symptoms is the first step toward managing them effectively. Seasonal allergies are often triggered by pollen from trees, grasses, and weeds, as well as environmental factors like mold, dust, and air pollution. Genetics and personal immune responses also play a role in determining susceptibility.
The good news is that natural remedies, preventive strategies, and dietary adjustments can significantly reduce symptoms without relying solely on medications. Lifestyle changes—like monitoring pollen levels, keeping your home clean, using air purifiers, and practicing good personal hygiene—are highly effective at minimizing exposure. Supplements, herbal remedies, and home treatments, such as saline nasal rinses, butterbur, quercetin, and steam inhalation, can calm the immune response and relieve discomfort. Additionally, an anti-inflammatory diet rich in fruits, vegetables, omega-3s, and proper hydration supports the body’s natural defenses against allergens.
While natural strategies are highly effective, severe or persistent allergies may require conventional treatments such as antihistamines, nasal sprays, or allergy shots. Combining natural and conventional approaches, when guided by a healthcare professional, provides the most comprehensive relief.